When Your Preemie Needs a Tracheostomy
by Richard and Cynthia Bissell
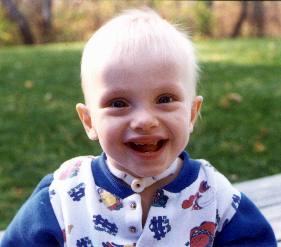 |
| Fifteen-month-old Aaron (a former 26-weeker) doesn't let his trach get in the way of his exploring and learning |
We will never forget the day we went into the hospital and found Aaron in respiratory distress. His little eyes were open wide with fear. As he gasped for breath he seemed to plead with us for help. We felt so helpless as we watched him struggle to breathe. We could hear a tiny squeak coming from him with every breath he took. He was immediately intubated.
It was difficult to remain calm as we listened to the rhythmic sounds of the ventilator breathing for Aaron at the same time the neonatologist talked. Aaron had subglottic stenosis (a narrowing of his airway). The doctor recommended a tracheostomy. The implications of this were enormous. We could not believe they were going to cut our baby’s throat. He was so tiny—only four pounds—and so fragile. We felt like we had been punched in the stomach.
Making a decision like this would be difficult under normal circumstances, but we were making it after weeks of little sleep and constant worry. We were forced to depend on the competence and integrity of the medical team. We were putting the life of our tiny precious son in the hands of strangers.
The most difficult part was kissing Aaron good-bye before sending him into the operating room. Part of us wanted to stop the whole thing and just hold him and tell him everything would be all right. Our more rational side handed him to the surgeon and watched tearfully as he was escorted down the hall.
Seeing Aaron for the first time after his surgery brought both relief and trepidation. He looked so much more comfortable: He was not struggling to breathe and he was peaceful. Yet, he had this foreign tube sticking from his throat and many tubes attached to his small body. We wondered, What would be the final outcome? Would he be able to talk? What would our lives be like as we cared for this child? Many of these questions could not be readily answered.
The day before Aaron came home from the hospital, the medical supply company delivered all the equipment we would need to care for him at home. Before we knew it, our living room was full of medical stuff—a suction machine, monitors, oxygen tanks, tubes, and wires. It was all a bit overwhelming.
Once Aaron was home, one of the scariest jobs was our first trach tube change without the backup of the hospital personnel. We were also afraid that his trach tube would become blocked or that a curious child (even Aaron himself) would pull out the tube.
Over time, trach care has become so routine that we often don’t think twice about it. To Aaron, the tracheostomy is just another part of him, like his eyes, ears, nose, and belly button. We try to treat Aaron as a typical kid, but with a few added precautions.
RICHARD AND CYNTHIA, MOTHER OF 26-WEEKER ERIC, TWIN TO ERIC
_________________________
"Your Premature Baby and Child," Helpful Answers and Advice for Parents, by Amy E. Tracy and Dianne I Maroney, R.N. Your Premature Baby and Child is one of the best preemie resources available today. Order your copy at: Amazon.com